Heart & Vascular Transcript
Heart & Vascular – James Higgins, MD Video
Opening screen with title “American Health Journal” and swirling graphics in motion.
[Serious music]
Announcer (V.O.): Heart disease is the leading cause of death in the United States. Over 600,000 people die of heart disease each year. At Valley Presbyterian Hospital, interventional cardiologist Dr. James Higgins reveals who is at risk for a heart attack.
V.O. visuals: Motion graphic of the vascular system of the human body, with zoom in to a close-up of the heart with blocked artery (images below);
.jpg)
.jpg)
(V.O. visuals continued) camera pan of Dr. Higgins walking along sidewalk of hospital toward the entrance.
[Music fades out]
James Higgins, MD: The risk for heart attack are many of the common factors I think that a lot of us are aware of and our doctors talk to us about every day. I’d like to split them up into what I like to say, modifiable risk factors and non- modifiable risk factors. So the non-modifiable risk factors would be sex.
Visual: Higgins being interviewed in a studio, wearing a shirt, tie and white coat, against a brightly colored abstract background. He is introduced with the title “James R. Higgins, MD – Valley Presbyterian Hospital” in the lower-third.
Higgins (V.O.): So, more common in male patients. Age, more common in more elderly or older patients. A family history of early cardiac disease…
V.O. visuals: Heavy men at an outdoor event walking toward camera; middle-aged man receiving a blood pressure test from a female nurse; close-up of blood-pressure cuff and stethoscope on his arm.
Higgins: …would also be a non-modifiable risk factor. Then you talk about a modifiable risk factor, which we all think about.
Higgins (V.O.): Hypertension. Diabetes. High cholesterol. Smoking, that terrible habit. Sedentary lifestyle. And obesity.
V.O. visuals: Close-up and camera pan of nurse administering a blood pressure test to patient; a senior male in his office testing his sugar levels; close-up of nurse writing on a vial of blood; close-up of fingers holding a lit cigarette; elderly woman sitting in recliner reading a book.
Announcer (V.O.): The symptoms of a heart attack are often not the same for men and women.
V.O. visual: Senior couple walking outside holding hands.
Higgins: Symptoms between men and women do vary. Men very commonly have a common presentation. Chest pain. (puts hand on his heart) Pressure-like.
Higgins (V.O.): Worse with exertion. It could also be at rest if it’s a certain type of heart attack or ST Elevation…
V.O. visuals: Female nurse checking and talking with middle-aged male patient who is touching his chest and describing the pain, as he lays on a gurney in the hospital.
Higgins: …Myocardial Infarction, the worse type of heart attack you can have. Women more commonly do present with vague symptoms.
Higgins (V.O.): Fatigue. Malaise. Weakness. Nausea. Vomiting. Maybe some shortness of breath. Maybe even wheezing. All of these could by symptoms of a pending heart attack and very important to pay attention to.
V.O. visuals: Middle-aged woman rubbing her eyes and forehead at computer; close-up of tired, young woman propping up her chin with her hand; camera pulls out to reveal her in a work cubicle dropping papers on floor; Higgins showing a male patient his heart on a computer monitor.
Higgins: Time is muscle. That means that the longer you wait, the more likely you’re going to have a bad outcome, even maybe death. So when you first feel signs of possibly a pending heart attack. Chest pain. Shortness of breath. Nausea. Dizziness. Anything that may be a concern for heart attack, especially if you are a person who has some of those risk factors we talked about earlier, then it’s important. The first thing to do…
Visual: Split screen with Higgins with “Chest pain,” “Shortness of breath,” “Nausea,” “Dizziness”.
Higgins (V.O.): …I’d say, is take an aspirin. It’s very important to chew that aspirin because we found out that by chewing that aspirin, it gets absorbed into your body that much faster.
V.O. visual: Extreme close-ups of aspirin tablets.
Higgins: And when I say time is muscle, I mean seconds. So, it’s very important to chew that aspirin and get it down as fast as you can. Next thing and probably one of the most important things that most people don’t do is…
Higgins (V.O.): …call 911.
V.O. visual: Split screen with an ambulance driving up to the hospital next to a red graphic with “Call 911” in white letters.
Announcer (V.O.): Dr. Higgins explains what a STEMI heart attack is.
V.O. visual: Close-up of heart beat on monitoring screen with the title “STEMI.”
Higgins (V.O.): STEMI, or ST Elevation Myocardial Infarction, or heart attack, is probably the worst type of heart attack that someone could suffer. These patients when they present to the emergency department are going to be in the most dire straights.
V.O. visual: The video continues with the words “ST-Elevation Myocardial Infarction” appearing under the title “STEMI”.
Higgins: The pathology actually that causes an ST Elevation Myocardial Infarction is actually a complete occlusion most commonly of…
Higgins (V.O.): …one of the major epicardial, or major arteries, that supply the heart with blood, and would be a 100% occlusion. These patients, if not tended to quickly, they could suffer great morbidity, and obviously mortality. A STEMI receiving center is something that’s been created by the government to help us to achieve our goals, which is to decrease mortality and morbidity from ST heart attacks, the worse type you can suffer. So, it’s a network of hospitals that have been branded with this…
V.O. visuals: Motion graphic of arteries with plaque areas that enlarge into a severe blockage (images below);
.jpg)
(V.O. visuals continued) health care worker preparing supplies in a cath lab; healthcare workers preparing a bed; a view of the receiving room with patient bed and special heart equipment; close-up of surgical and medical supplies; Higgins looking at computer monitor next to receiving room, displaying patient’s heart beat and blockage; close-up of his hand on a monitoring console.
Higgins: …designation. And, at all these hospitals basically, you have a 24-hour cath lab, which provides you with…
Higgins (V.O.): …the most important therapy, (inaudible) aspiration for opening up that occluded artery and you have highly trained personnel who is on call 24 hours a day, including myself, an interventional cardiologist, is ready to work at a moment’s notice to be there to save your life and to help you have the best outcome possible. Now a patient may come in and we vascularize them, we open their blood vessels up…
V.O. visuals: close-up of a lab worker holding stent supplies; Higgins at monitor continuing to review the patient’s heart and arteries; close-ups of blocked blood vessels.
Higgins: …they feel great and are ready to go home the next day and they think ‘I have a new lease on life and I’m going to go back to all my bad habits and do everything again.’ But in reality, it’s a spectrum. So, this process could continue to happen in your vessels and if you’ve proven to me you can do it once, I know you can do it again.
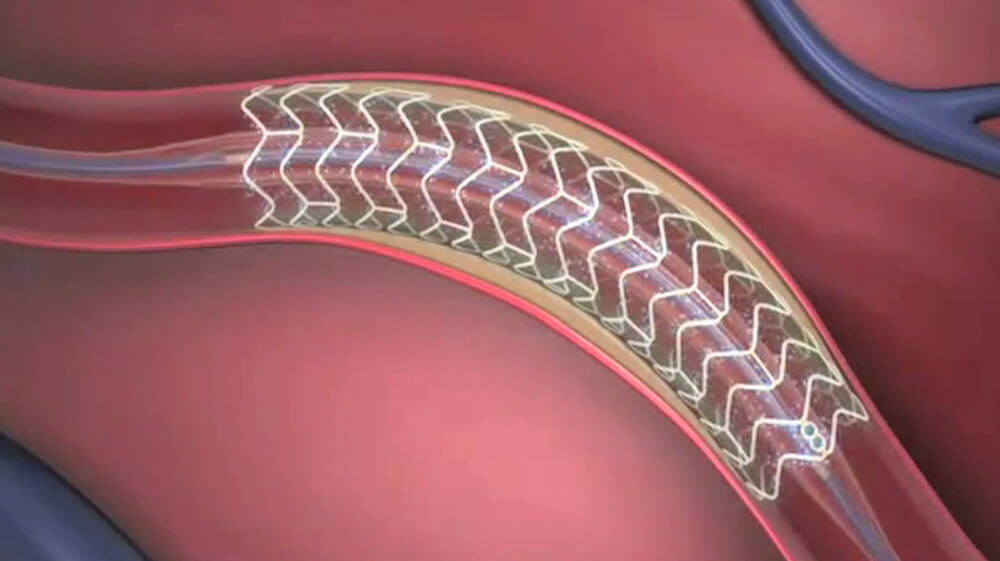
Higgins (V.O.): So it’s very important to stay on point, to take your medication that’s prescribed to you to help to keep these vessels open and importantly to help keep one of the devices that we put inside of your body called a stent, which helps keep your vessel for the long-term, to help keep that stent open, keep the vessel (inaudible) for you.
V.O. visuals: Elderly man taking his medication; motion graphic of blood flowing through partially blocked artery and tubular stent inside the artery, expanding to open it up (images below).
Announcer (V.O.): Dr. Higgins discusses the satisfaction in helping patients.
V.O. visual: Higgins being interviewed in the studio.
Higgins (V.O.): Being a cardiologist and especially an interventional cardiologist is somewhat of a dream, honestly…
V.O. visual: Higgins in the cath lab holding stent supplies;
Higgins: …because you can affect people on two different levels. There’s the initial level where today I’ll go to my office and I’ll see patients and I’ll give them preventative care and I’ll treat those modifiable risk factors (shakes finger at camera, smiling).
Higgins (V.O.): I’ll treat their high blood pressure, their high cholesterol. I’ll talk to them about smoking. Then there is the other half of it. The half where I’m called in the middle of the night and a patient is suffering a STEMI. So for me, to be able to come in the middle of the night and know that this patient was suffering the possibility of death…
V.O. visuals: Higgins at his office computer with male nurse looking over his shoulder at heart images on the screen; close-up of Higgins studying the images.
Higgins: …and when I see their face and I know that they’re terrified and they think that this is going to be it. And, after I finish opening their vessel, to see the happiness in their face, to see the relief in pain, to see the happiness in their family, honestly there’s not a better feeling when you have somebody’s husband, somebody’s wife, somebody’s daughter. They hug you, they cry, and they understand the importance of what you just did to save their family member.
Visual: Higgins being interview in the studio.
End screen is black.

