Strokes Transcript
Strokes – Brian Ostick, MD Video
Opening screen with title “American Health Journal” and swirling graphics in motion over blurred images of physicians.
[Serious music]
Announcer (V.O.): According to the CDC almost 800,000 people suffer a stroke each year in the United States. On average, one American dies from a stroke every four minutes. Dr. Brian Ostick at Valley Presbyterian Hospital discusses the symptoms of a stroke that indicate immediate medical intervention is needed.
V.O. visuals: Centers for Disease Control and Prevention (CDC) exterior sign; split screen graphic with an illustration of the human brain, blood vessels and spinal column opposite the descriptive text “Almost 800,000 people suffer a stroke each year in the United States”; an ambulance turns into a hospital entrance toward and past camera; Dr. Brian Ostick in front of a monitoring machine in the ER talking; exterior of hospital; exterior “Emergency Entrance – Basic Emergency Medical Service Physician on Duty 24 Hours” sign.
[Music fades out]
Brian Ostick, M.D.: Symptoms of a stroke can be varied. Some of the most common are a facial droop, arm weakness, and slurred speech. And so we use a mnemonic called FAST, F – A – S – T, and that stands for F for facial droop, you can see the face drooping to the right or the left side of the face. Arm weakness is the A, and if you could ask somebody, or a loved one, or a friend whose potentially having a stroke to hold their arms out like this with their palms up. (He outstretches his arms in front of him with his palms upward.) And if there is one that would drift to the side like this (he drops each of his arms separately downward toward his side) then that would potentially be a sign of a stroke because there is weakness in one side of the body or the other. And then the last is slurred speech, so if somebody normally speaks very clearly and then all of a sudden their speech becomes garbled or difficult to understand that could be another major sign of stroke and that’s the S. The last part of the FAST mnemonic is the T and that stands for time. So if you see any of those signs of stroke, facial droop, arm weakness…
Visual: Close-up of Ostick in a suit and tie, being interviewed in the studio against a brightly lit gray background. He is introduced with the title “Brian Ostick, MD – Valley Presbyterian Hospital” in the lower- third. On the top right of the screen, the FAST list appears: “Facial droop,” “Arm weakness,” “Slurred speech,” and “Time” progressively listed under it.
Ostick (V.O.): …or slurred speech you want to act fast, so you should call 9-1-1.
V.O. visual: Ambulance passing by camera on busy city street and turning into a hospital entrance.
Announcer (V.O.): Dr. Ostick explains the two types of strokes.
V.O. visual: Ostick in ER talking with another physician behind the desk.
Ostick (V.O.): There is ischemic stroke, meaning there is a blood clot in the brain that the blood can’t get past. So the brain cells that require oxygen to function aren’t getting that oxygen anymore that comes from the blood. So that’s a blood clot, an ischemic stroke. There’s another type of stroke called hemorrhagic stroke where you have actual bleeding inside the brain itself and so that type of stroke, unfortunately, usually will need surgery to repair it, try and stop the bleeding at where it starts. Both of them are very dangerous and very serious. Both of them can be tough to treat but they do have totally separate treatments, whether it’s an ischemic stroke versus a hemorrhagic stroke. Sometimes we see people…
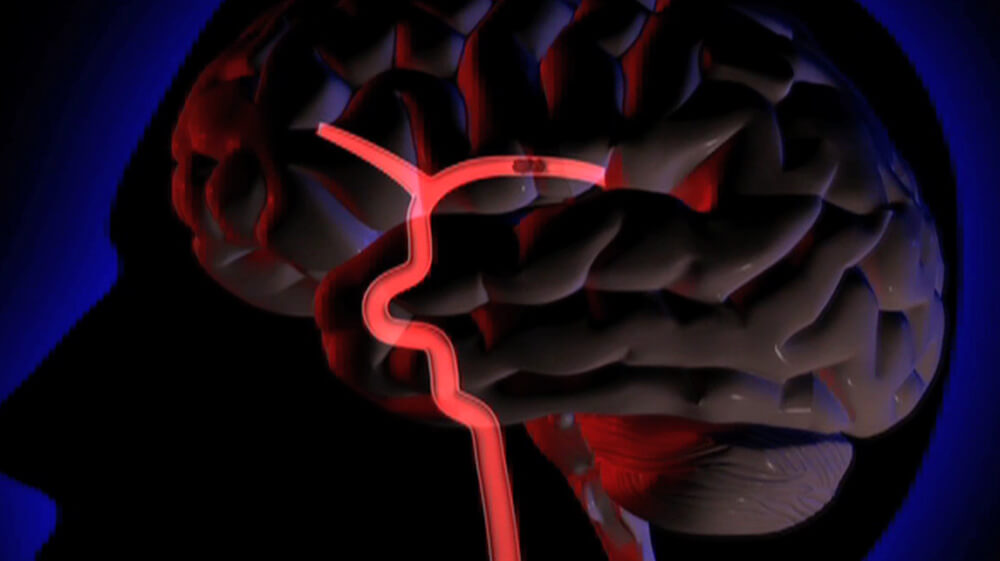
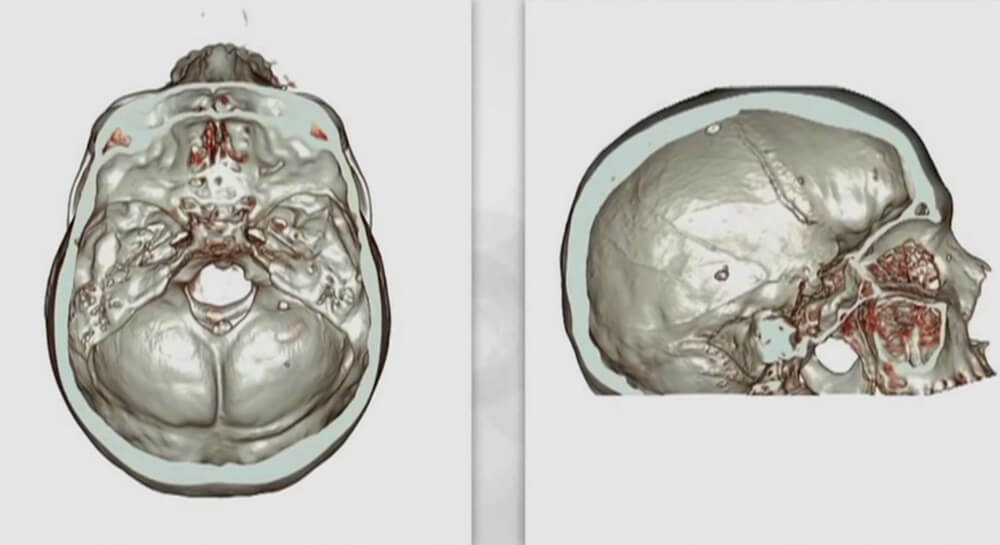
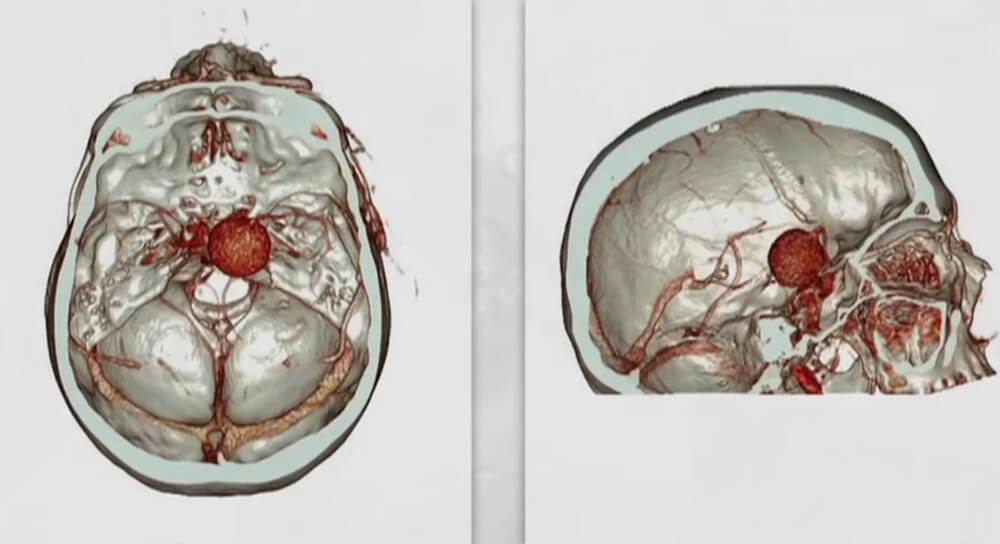
V.O. visuals: Motion graphic illustration zooms in to show a blockage in a blood vessel in a human brain; another motion graphic of the brain, blood vessels and spinal column zooms in to show the blood vessel discolored as it no longer gets blood and oxygen (images below).
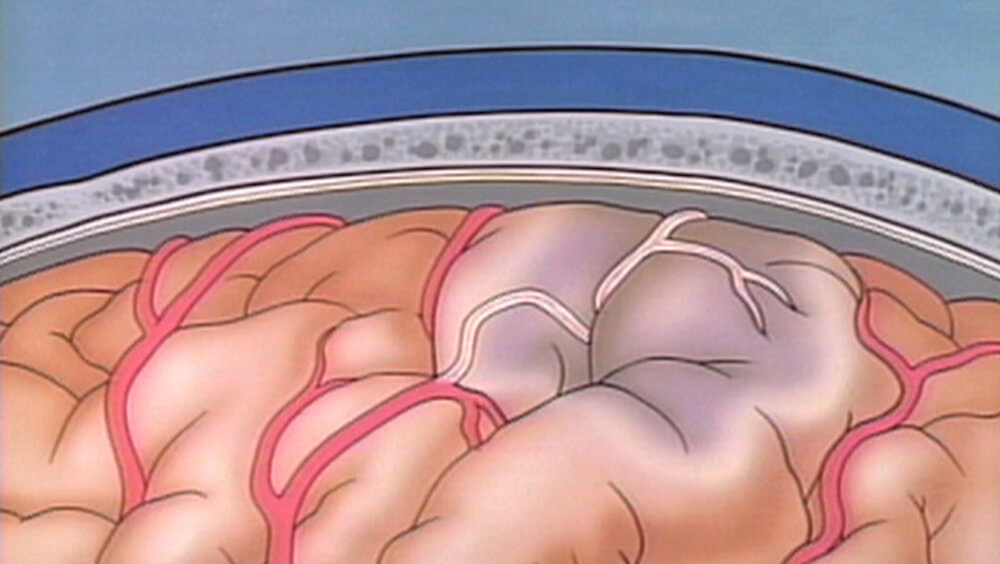
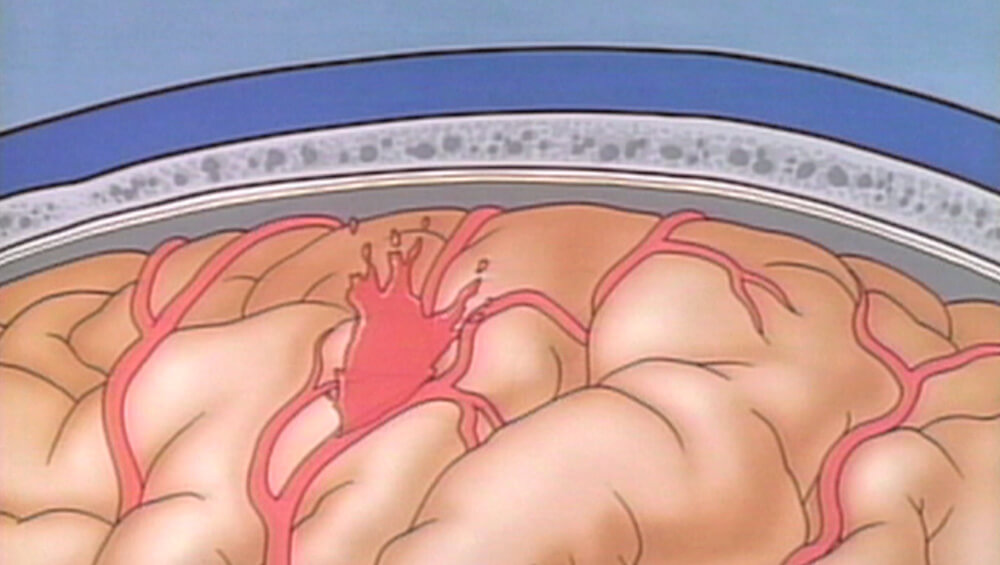
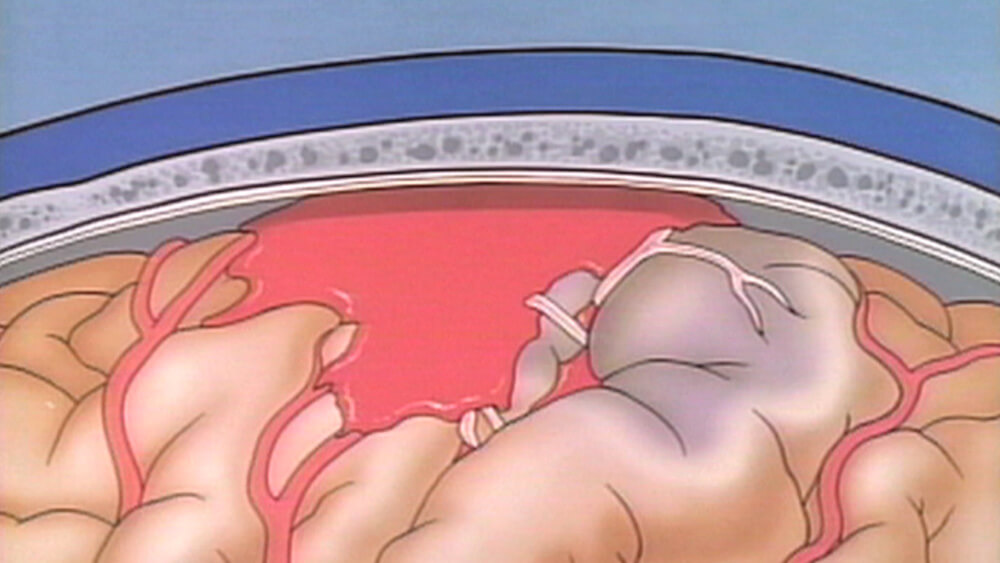
(V.O. visuals continued): inside of a radiology room with a brain scan displayed on a large monitor; close-up view of the scan showing a hemorrhagic stroke; a female doctor at a desk points to a computer monitor that displays a hemorrhagic stroke; motion graphic illustration of blood pouring from a blood vessel and pooling inside the brain (images below):
(V.O. visuals continued): Ostick talks to a male nurse in the ER and then turns to talk with another doctor while viewing a computer monitor.
Ostick: …that come in with symptoms of a stroke like the facial droop or numbness and tingling or weakness and that’s resolved by the time they get to the ER or resolved in the first twenty-four hours, and that can be something similar to a stroke called a TIA or transient ischemic attack. We treat those very seriously too because people with transient…
Ostick (V.O.): …ischemic attacks can sometimes go on in the next twenty-four to forty-eight hours to progress to a full stroke.
V.O. visual: Another angle of Ostick and the other doctor as they continue to look at the monitor.
Announcer (V.O.): Getting prompt treatment for a stroke increases chances for a better outcome.
V.O. visual: Split-screen motion graphic illustration of a normal brain and one with a hemorrhagic stroke (images below).
Ostick (V.O.): If we identify somebody with a stroke and they are within the window that we can give them medicine called TPA, which is a very powerful blood thinning medicine, then we call what we call our ‘Code Stroke’ and that brings our entire team to the bedside of the patient. It’s the doctor, the nurse...
V.O. visual: Female doctor and a team working on a female patient on a gurney in the ER.
Ostick: …the radiology tech, the laboratory team, and things happen very quickly because we have, up until about four-and-a-half hours from the onset of the stroke to give this medicine called TPA. And once you’re past that four and a half hour time window, it’s too dangerous…
Ostick (V.O.): …to give that medicine. The sooner you can get that TPA on board, the safer it is for the patient and the better chance you have of reversing those symptoms of the stroke.
V.O. visuals: Ostick continues viewing monitor and talking with the doctor in the ER; several large monitors in a room display brain scans; close up of a scan with a blood clot.
Announcer (V.O.): Specialized techniques can be used to deal with the source of the stroke.
V.O. visuals: Another view of a rotating scan with a blood clot; Ostick in front of a monitoring machine in the ER talking.
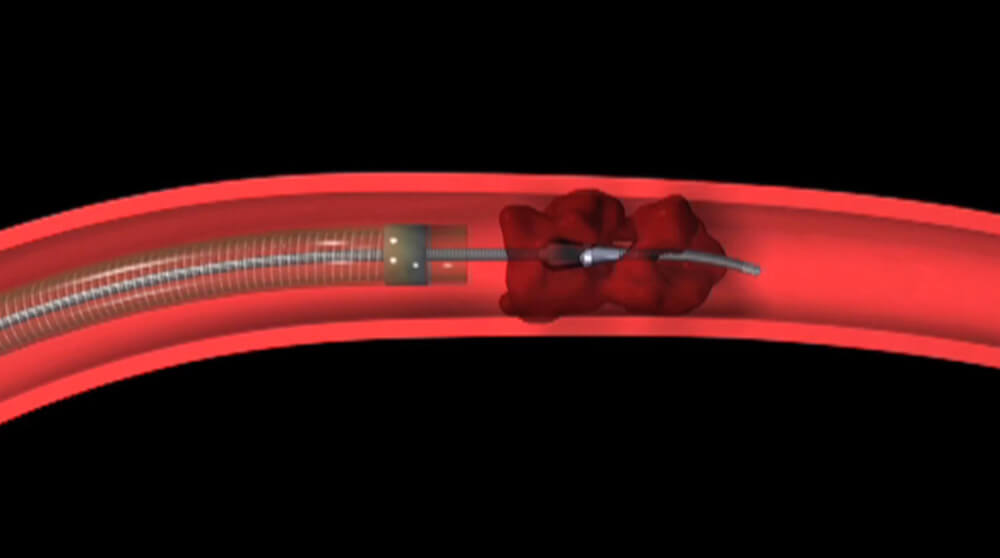
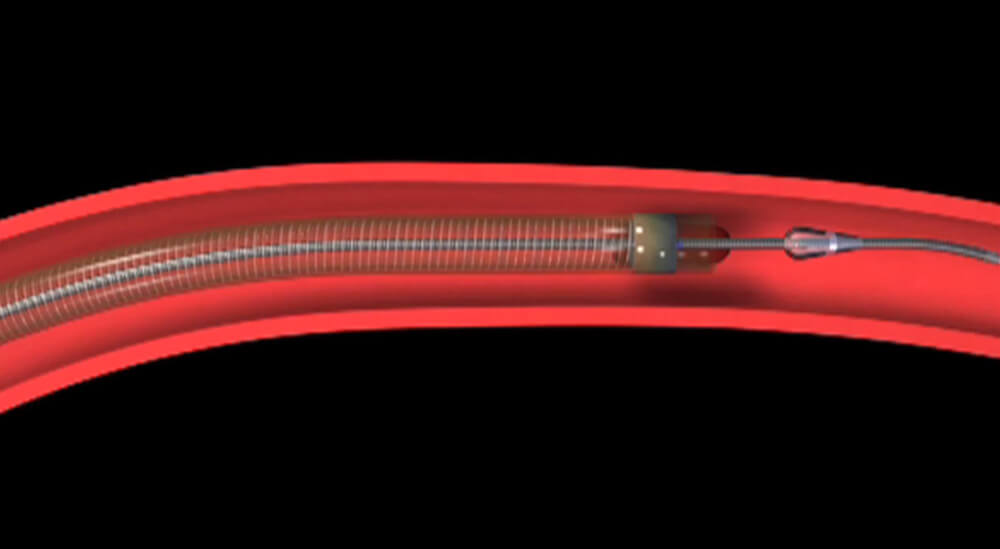
Ostick: In very specialized centers, go in with a catheter, go directly to the point of the clot, with a small wire and tube…
Ostick (V.O.): …and be able to deliver the TPA directly to the clot or potentially even put a coil through that clot and pull it out. And so that’s very specialized treatment that is done at something called a comprehensive stroke center.
V.O. visuals: Motion graphic of a wire on the end of a coil tube inserted through the center of a clot and then encasing it as the coil pushes through the blood vessel (images below).
(V.O. visuals continued): Ostick walking through ER unit toward and past camera.
Ostick: Not every hospital is equipped to do those sorts of procedures but that is an option up to eight hours from the onset of the stroke.
Visual: Ostick being interviewed in the studio.
End screen is black.

